AI
Discharge instructions that patients are motivated to follow
Many patients find it challenging to read through the 10-15 pages of discharge instructions they receive, and a significant portion may end up discarded
Discharge instructions that patients are motivated to follow
Many patients find it challenging to read through the 10-15 pages of discharge instructions they receive, and a significant portion may end up discarded.
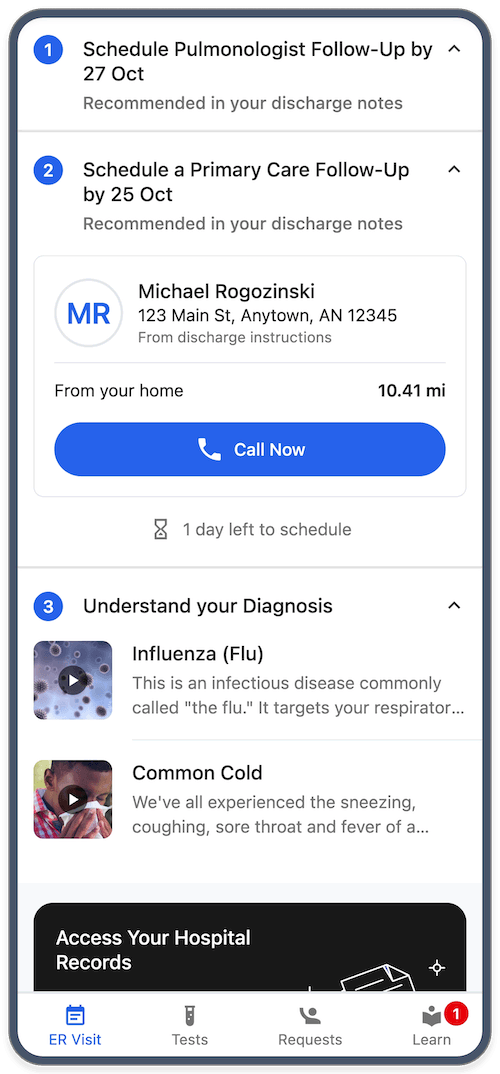
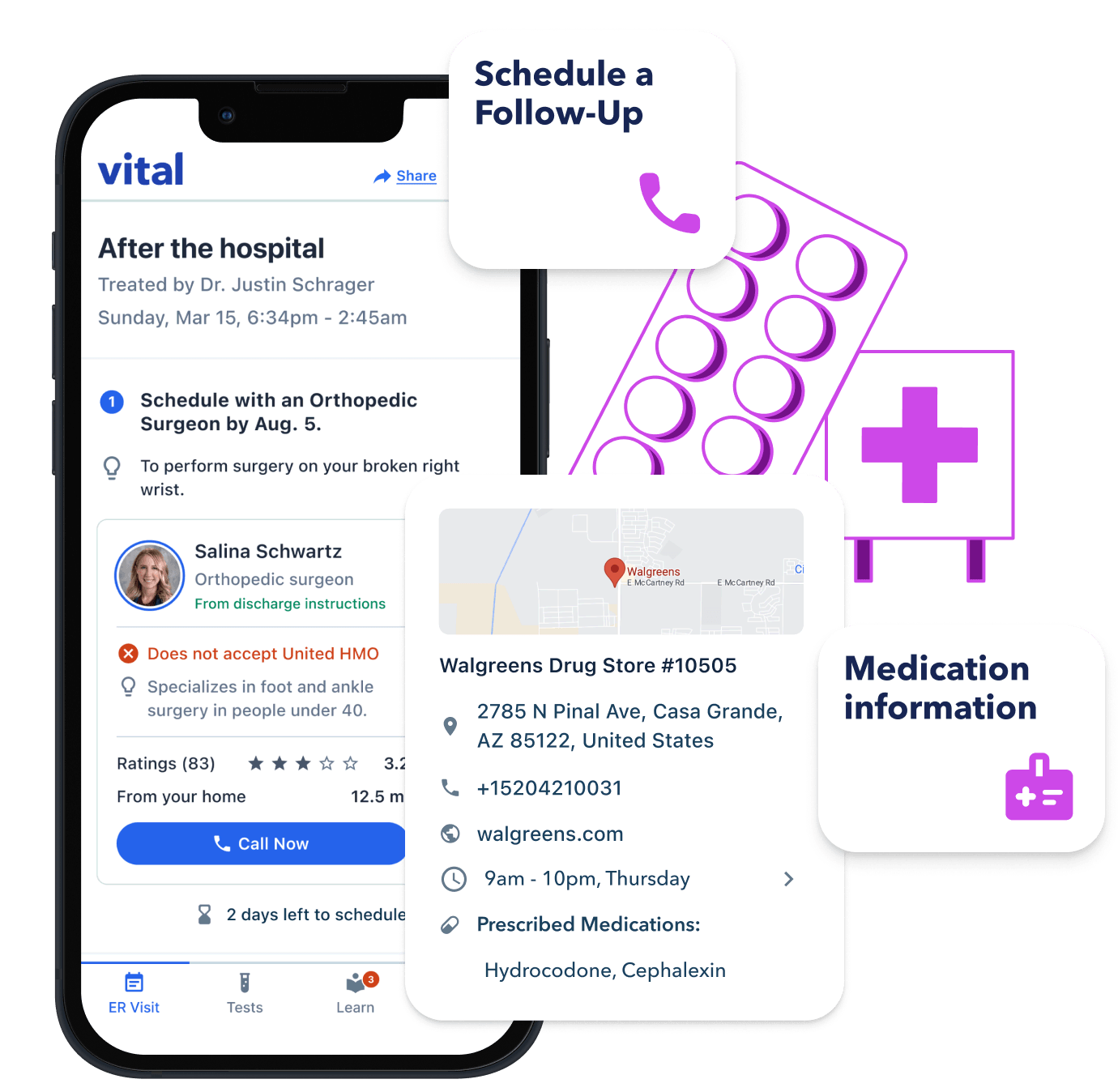
Vital uses AI to parse discharge instructions into a 1-2-3 step checklist.
Vital summarizes the “to-do list” in discharge instructions for higher adherence to plan, resulting in lower readmissions and better health outcomes. This includes:
An AI summary of their medical plan & assessment.
Follow-up appointments with due dates for each.
A list of new medications, which pharmacy they were sent to, and pharmacy hours + directions.
Tertiary task list: sign-up for the patient portal, give a nurse compliment, and watch videos on diagnoses.
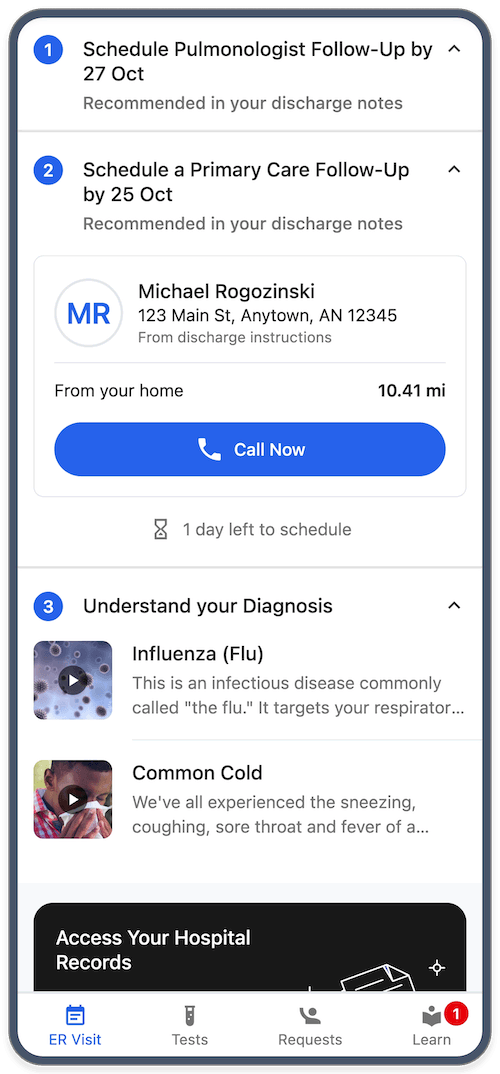
Discharge documentation comes in many different formats, and much of it is boilerplate. Vital uses generative AI to parse discharge paperwork into:
A quick paragraph summary of what the patient diagnosis was, what to do or not do, and when to return to the hospital.
Follow-ups (including multiple specialist and PCP follow-ups)
Medication changes, new medications, and which pharmacy an Rx was sent to. We then lookup store hours and driving directions in Google Maps.
Diagnoses, which are automatically matched to education
Vital’s AI automatically handles many variations of discharge report with little to know configuration. That means whether you use EPIC, Cerner, Veradigm, Meditech, or some combination of EHRs, we have you covered.
