AI
AI can find a needle in the haystack
Incidental findings are those outside of what was primarily being looked for during radiology imaging
95%accuracy across modalities
+5FTEs returned to care
+$800knew radiology follow-ups
AI can find a needle in the haystack
Incidental findings are those outside of what was primarily being looked for during radiology imaging. For example, you might be looking for a ruptured appendix (primary emergency) and just so happen to see a nodule on a kidney nearby. While not life threatening today, these findings need to be re-evaluated and tracked over time to make life saving decisions for our patients.
Today, 83% of incidental findings have no scheduled follow-up. That’s a big loss in hospital revenue, and also a big loss for patients: if it is cancer, it could have been caught early.
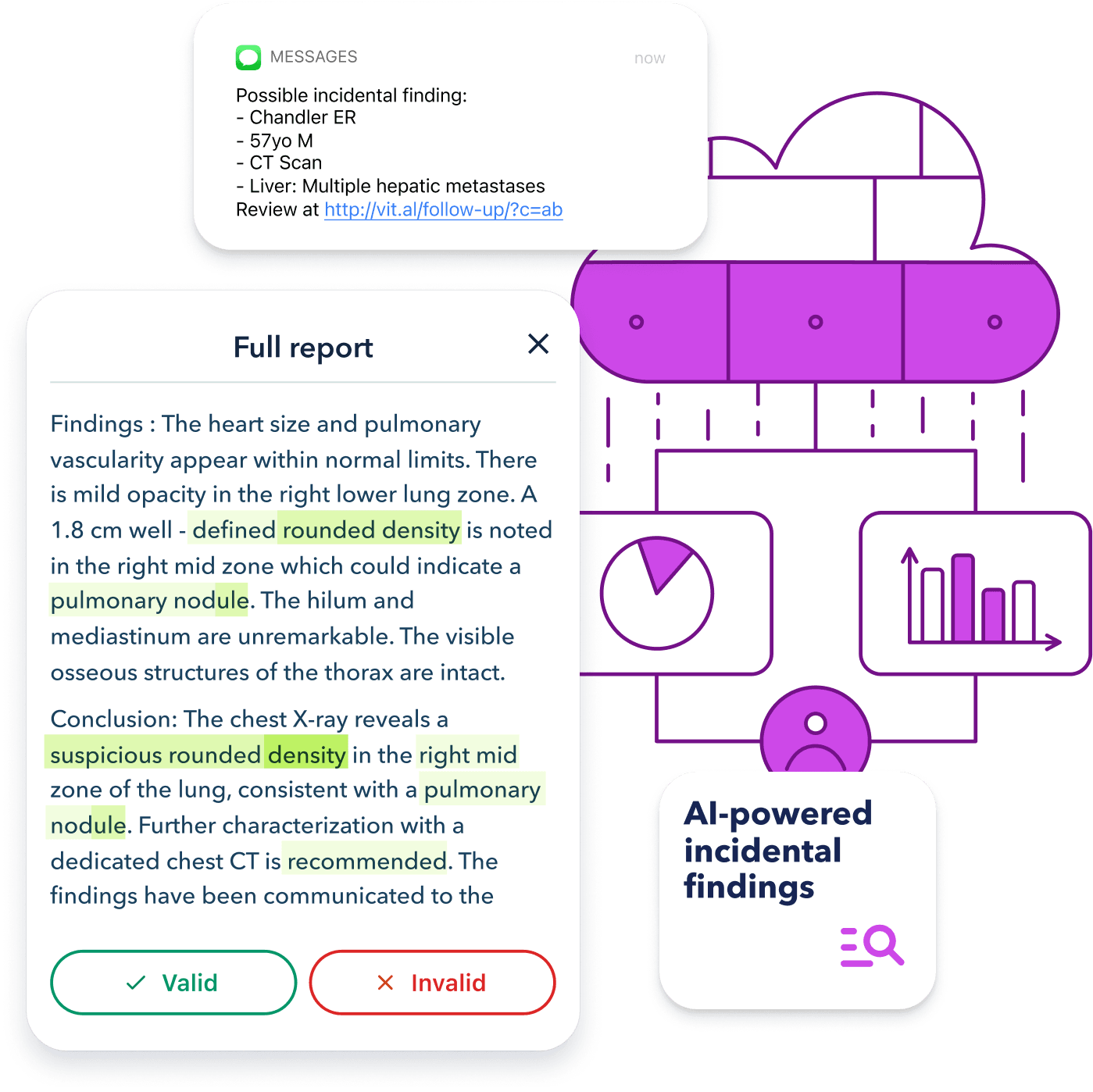
Vital uses advanced natural language processing AI on the text of radiology reports to detect the 7-15% rate of incidentalomas. That’s far faster than a manual review.
Identify all the incidental findings with advanced AI
Vital uses language models custom trained on long clinical text to identify:
Neoplasms
Cardiovascular & peripheral vascular disease, aneurysms
Asymptomatic hypertension
Other non-acute but important findings
Vital Guard makes identifying and communicating incidental findings simple, consistent, and easy
Incidental findings in Radiology studies are very common in the hospital. In some patient groups, the rate can be as high as 35%. Overall, 1 in 12 of your ED patients will have a new incidental finding, but, shockingly, only 10% will learn of it from their care team. This poses a massive problem for clinical outcomes, patient experience, and medical-legal liability.
Dramatically reduce the work load of the after care team
Vital Guard is the solution to this problem. Incidental findings are identified in near-real time and added to a list for clinical review. A single staff member, or multiple staff members can easily monitor a single facility or an entire health system on the same screen–keeping your team working at the top of their license with efficiency and effectiveness. Our tool not only calls out incidental findings that were not disclosed during the patient encounter, but we have a suite of tools that allow for asynchronous patient outreach and verification…no more sitting on the phone.
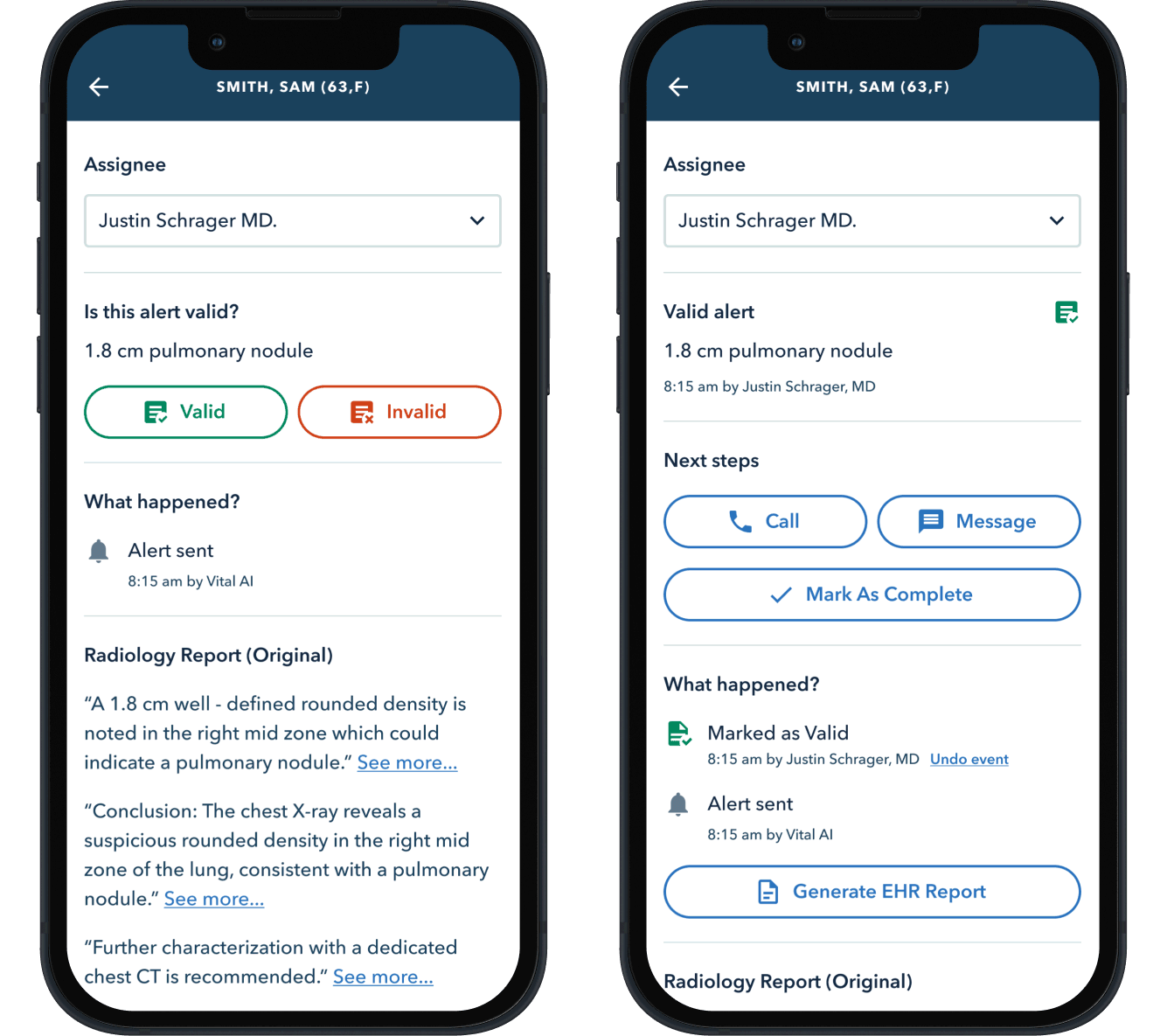
Streamlines patient contact
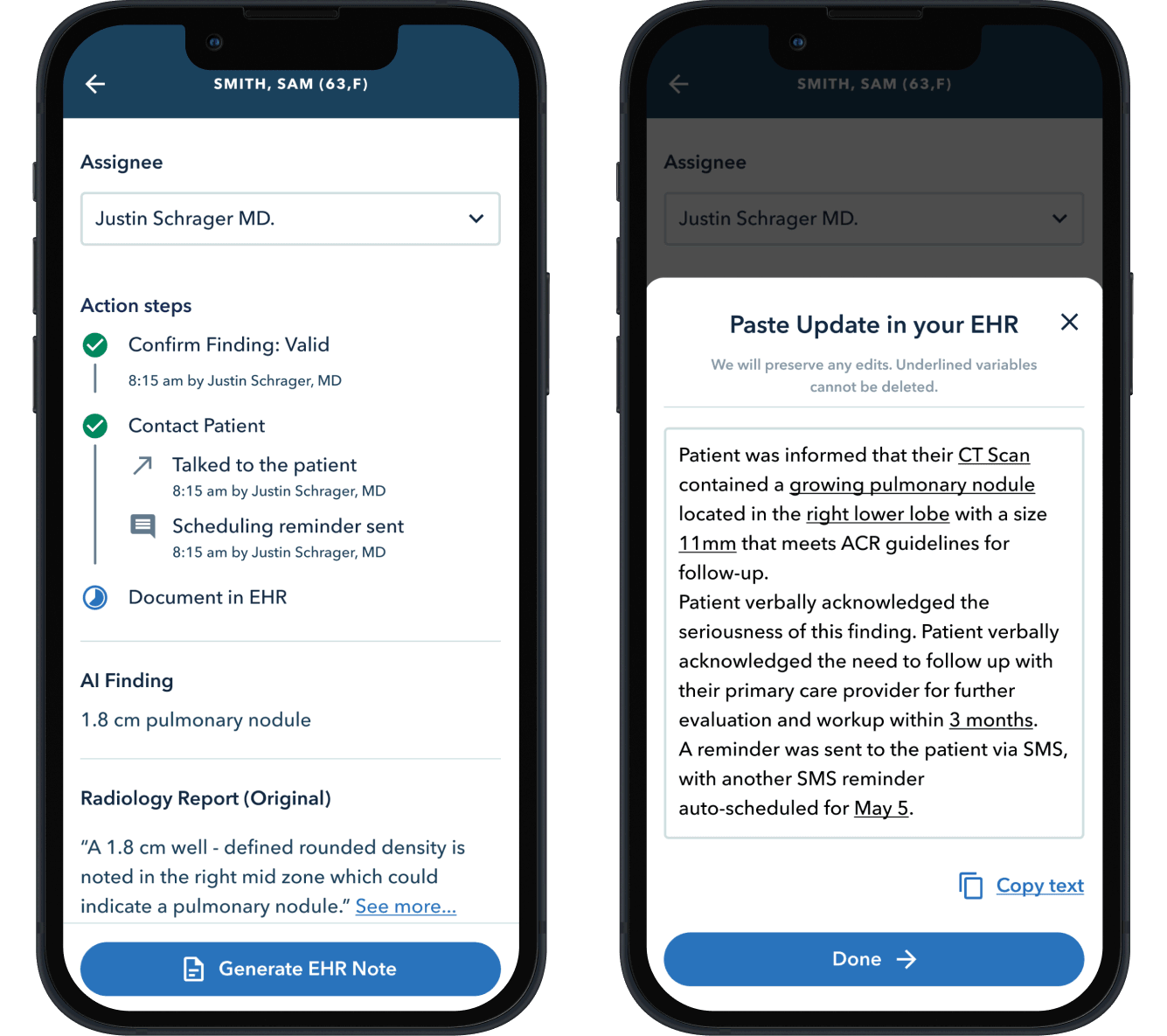
Once an incidental finding is confirmed, it’s required that a provider explain the seriousness of an incidental finding to the patient, and document the patient’s understanding. There are several possible scenarios:
Patient answers the phone and speaks to a provider
EHR text is auto-generated for documentation
In person follow up while the visit is active
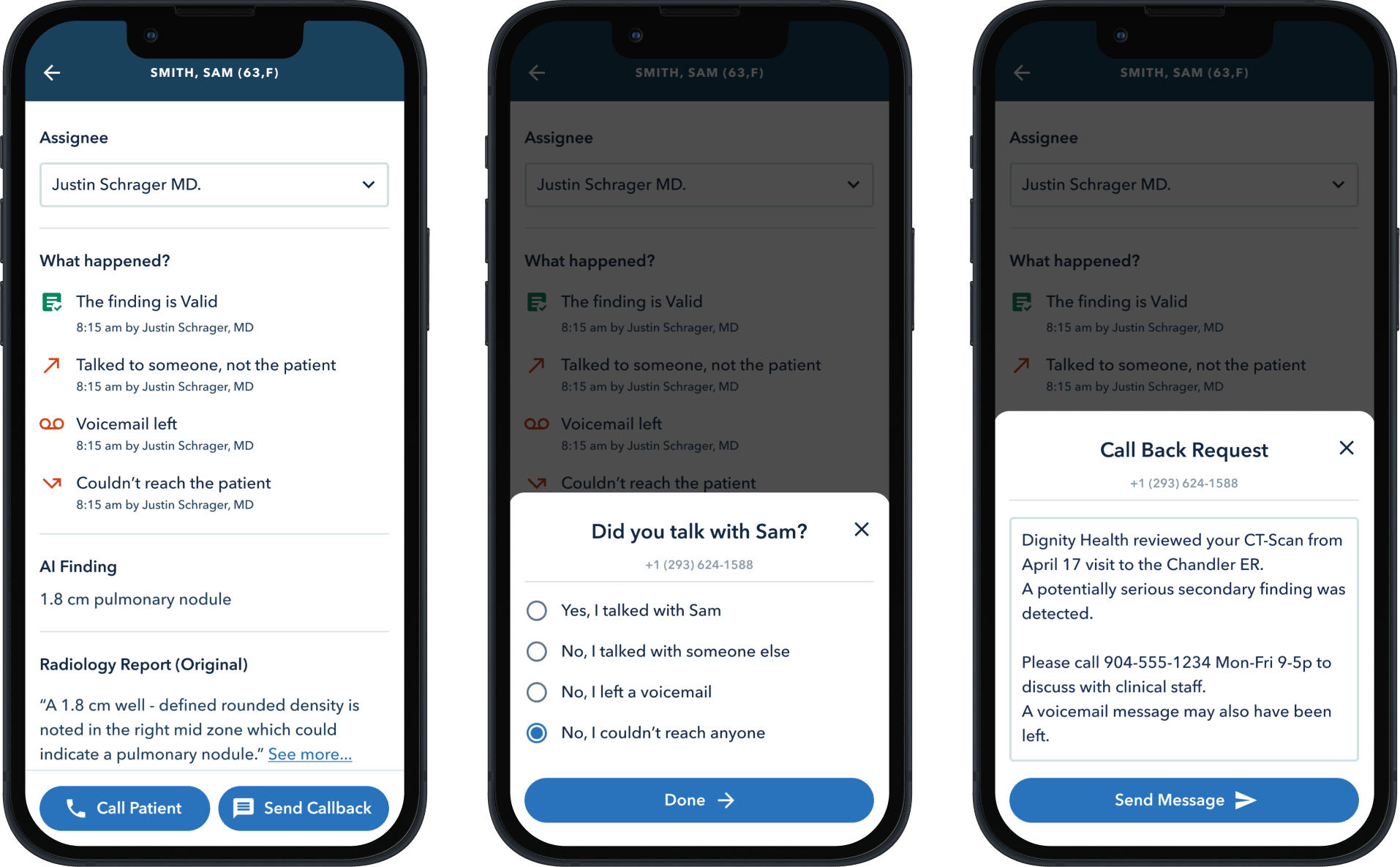
Even for hard-to-reach patients
Only ~20% of patients answer calls from unknown numbers. A better approach is to request a call-back using a serious, but not-too-ominous text message. While these can be edited if a provider wishes, all of this communication happens with just a click or two.
Case Study: Patricia, 73
Patricia, 73, had imaging that incidentally revealed a thoracic aortic aneurysm. When I contacted her, she already had an upcoming appointment with a cardiothoracic surgeon for management of her known valvular heart disease. Yet, she was unaware of the aneurysm. This presented a perfect opportunity for her to discuss the incidental finding during her scheduled visit. I explained the importance of monitoring the aneurysm and encouraged her to bring it up with the specialist. She expressed gratitude for this new awareness, adding to her preparation for the appointment.
This common scenario illustrates how our program enhances, rather than duplicates, ongoing specialty care by empowering patients with important information.
Case Study: Marcus, 54
Marcus, a 54-year-old man, was seen in the ED for back pain with pain radiating down his right leg. A CT scan revealed an incidental left adrenal mass noted as an incidental finding. The mass was communicated in the body of the report and via secure message, but outreach required follow-up context to ensure the finding was understood and acted upon.
Our AI-assisted workflow flagged the incidental adrenal lesion and prompted outreach.
An initial secure message on 12/16/2025. Our systems showed the patient had viewed the message. A second contact attempt was made by phone on 12/18/2025. I spoke with Marcus to review the significance of the finding and recommended follow-up. He was appreciative of the call, confirmed he had viewed the secure message. As a result, he reported he had already contacted his primary care physician and been referred to endocrinology for consultation and monitoring.
This case highlights how important incidental findings can be overlooked without active follow-up—and how a structured communication program helps patients receive timely evaluation and care.
Case Study: Bob, 83
Bob, an 83-year-old man, underwent a CT scan of the abdomen for evaluation of abdominal symptoms. The imaging incidentally revealed a thoracic aortic aneurysm measuring 4.2 cm. He was not admitted, and when outreach was initiated, Bob invited his wife to join the discussion. As Bob’s medical power of attorney (MPOA), his wife manages his medical records and coordinates his care. She is a retired nurse and appreciated the opportunity to review the findings.
During the conversation, the incidental finding was clearly explained, along with instructions on how to obtain a copy of the radiology report. Bob’s wife indicated that she would discuss the finding with Bob’s established cardiologist at an upcoming appointment. Both Bob and his wife expressed appreciation for the clear guidance and felt prepared to address the finding proactively.
This case highlights how involving care partners, particularly those who assist with medical decision-making, supports effective communication and helps ensure that important incidental findings are appropriately addressed.
Reduction in medical-legal liability
Many patients are self-insured (Emory, Envision).
Malpractice premiums are increasing.
The trend seems to be that malpractice caps are going away.
Statute of limitations are being increased for specific conditions (cancer).
A new source of radiology revenue
Today’s ~30% incidental finding follow-up rate can be increased. For an average hospital with 200 beds and 50,000 annual ED visits, we might expect 150,000 radiology reports, 10k of which have some incidental finding.
+20% x 10,000 incidents = 2,000 incremental new radiology orders
x $400 / radiology order
= +$800k
Good for patients
ACR & ACEP recently appointed a committee to recommend best practices, which underscored the importance of incidental finding communication, patient-facing language, and tracking systems…
Actionable incidental findings are common in emergency department imaging and present unique challenges in reporting, communication, and ensuring appropriate follow-up … standard practices for communication between clinicians and patients and among clinicians are important when actionable incidental findings occur in emergency department imaging … communication and follow-up of actionable incidental findings in emergency department imaging represent a systems issue that can be enhanced through use of informatics and tracking systems. - Moore et al. 2023
